As we head into November, which is Lung Cancer Awareness month, I wanted to give a general overview of data from this year showing the important link between Major Cardiac Events and Radiation Dose to the heart.
To me, I think it is amazing that there are this many studies from this year. This isn’t old “historical” data from the ’90s – this is all current 2019 data. It’s amazing that I can easily put together this volume of brand new information on the connection between heart radiation dose and cardiac events. (Sometimes I laugh at how often physicians still quote studies from decades ago – but that is a different story).
This blog post was inspired by a press release (shown below) written by Anicka Siachta. I had seen the original medical study at ASTRO and had used the data to reply online in several different ways, but the report below, for whatever reason, came across with great clarity and focus. Once I read the summary below, I knew I needed to help compile a more robust set of current data as we head into Lung Cancer Awareness Month. First, here is the article that inspired this post.
The Effect of Radiation on the Heart
It’s really a great summary of the article and it covers the important data very well – well done on the write up! Here is the main graph of the article that drives home a few points.
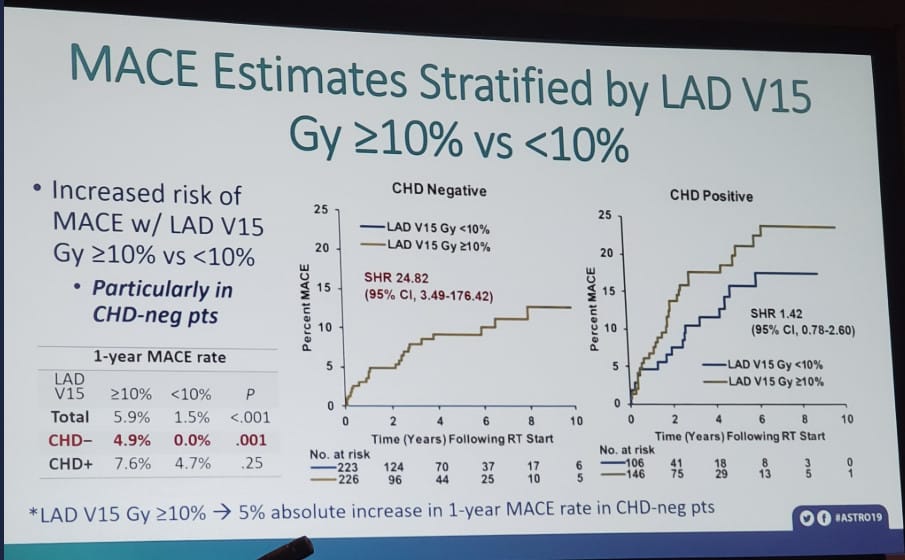
Focus on the upper right-hand outcome box (B). These are people with NO history of Coronary Heart Disease. Just THREE years after a radiation dose of 10 Gy to the heart, ~5% of patients have had a MAJOR Adverse Cardiac Event. 1 in 20 in just 3 years. Those really are crazy (bad) numbers. Lower heart radiation dose resulted in significantly fewer cardiac events.
The other curves show that people with and without heart disease have cardiac events, and (my interpretation) it’s harder to find a link in those with pre-existing heart disease due to the high number of events we see after radiation to the chest – i.e., in the group at high risk for having an event, it is statistically harder to prove that something changes that baseline risk (just based on math).
So that is the inspiration – At just 3 years – 5% more patients with lung cancer suffered major cardiac events because of radiation dose to the heart when the heart was not avoided.
As reported, that is a modifiable risk – i.e. your treatment team can do things to reduce heart dose.
How to Reduce Radiation to the Heart during Treatment
The two main pathways in radiation oncology today to reduce heart and coronary risk over IMRT/VMAT from my perspective are breath-hold techniques and proton therapy. It’s a bit beyond the scope of this article today to go into the differences between these approaches, but both are effective in various scenarios. In general, they reduce normal tissue radiation across a wide spectrum of cancer treatments, and both have places where they are home-runs (my opinion).
To me (and I’ve treated with both), Proton Therapy is the more robust path to reduce heart dose – especially beyond simple tangent breast treatments (breath-hold is very good there). It works in difficult cases where breath-hold techniques can’t dramatically reduce heart dose. It works because protons stop and x-rays don’t.
Proton Therapy pretty consistently allows for a lower dosage to normal structures. There really is very little doubt in many cases. The medical argument then becomes a cost/benefit argument, or which cases benefit the most. Just to show a few more studies for lung cancer that show links between Mean Heart dose and Major Adverse Cardiovascular Events or Heart dose and Reduced Overall Survival. These are two more studies presented this year showing that heart dose in the management of lung cancer is a point of research.
The main cancers where protons often deliver significantly less heart dose are:
- LUNG CANCERS WITH TUMORS IN THE LOWER PART OF THE CHEST (NEAR THE HEART) – TUMORS AT VERTEBRAL BODY T7 AND BELOW.
- COMPREHENSIVE BREAST CANCER TREATMENT – BOTH LEFT AND RIGHT BREAST CANCER CASES – LEFT GREATER THAN RIGHT
- LYMPHOMAS OF THE CHEST – LOWER IN CHEST, FEMALE PATIENTS, HEAVILY PRETREATED CHEMOTHERAPY PATIENTS
- ESOPHAGEAL CANCERS – MAIN BENEFIT IS MID TO LOWER ESOPHAGUS. HIGH CHEST TUMORS BENEFIT THE LEAST WITH RESPECT TO REDUCING HEART DOSE.
The Effect of Radiation on Patients with CAC
Here’s another broad group of patients where monitoring heart dose appears critical – patients with Coronary Artery Calcium (CAC for short).
First – what is CAC? Basically, it is calcium in the main heart arteries that shows up on a simple CT scan. Every time you have a radiation simulation these days, you’ll have a CT for planning. CAC in cardiac literature requires some special series, but here is a simple example of calcium in the arteries of the heart that you can easily see in a radiation oncology clinic during treatment planning.
According to data, the above patient is at MUCH higher (10% higher in fact) risk of DEATH in the first 2 years following chest radiation. Below is the study – again presented just this year.
And it’s not just whole heart dose that matters. (That makes sense.)
The more we study the heart, the more we learn that different pieces of the heart are particularly important. Makes sense – some parts of the heart are more important.
So why do we, at the Oklahoma Proton Center, often talk about Mean Heart Dose? To put it simply, you have to start somewhere to raise awareness. The simple story that the whole heart should get a low dose of radiation is easy. So we often start there, but there are more things we monitor to try to maximize outcomes.
In the picture above, the vessel highlighted with the red arrow is the LAD – the Left Anterior Descending Coronary vessel. Its nickname in public literature is “The Widow Maker” because a block in that artery often leads to fatal cardiac events. The more we learn, the more we are sure that reducing radiation to this blood vessel is important. Here’s another study from this year looking at dosage to the LAD.
This study shows that lower doses to the LAD resulted in a 5% difference in Major Acute Coronary Events at 1 year. Radiation to the heart causes a significant number of additional events very early after treatment.
What should heart dose be? I tend towards the simple answer: Less is better. We shoot for <1 Gy to the heart as a starting point. We also monitor dose to the LAD and keep it low according to the paper above (technically using V15 to less than 10%).
Proton doses are VERY different in places than traditional IMRT plans. Sometimes, we can’t reach a low dose like <1Gy – such as for some esophageal cases or for some large-volume lung cases – but in many cases, we can. The literature for breast cancer treatment is some of the more robust, and in many series, published doses of proton therapy are about 1/15th the doses that can be achieved with IMRT.
TAKE HOME: Radiation dose to the heart is a modifiable risk. For a number of cancers in the chest, proton therapy can dramatically reduce the radiation to the heart. Data is piling up that says this should result in fewer cardiac deaths from radiation damage.
Like I say repeatedly in this blog, you must be an advocate and ask about your options. There is no good way that I can tell you over the phone or via the internet that your plan would or would not be better with protons. I can make educated guesses, but to me, you need to have a side by side comparison of both approaches for your cancer treatment. That comparison cannot be created at a facility that doesn’t offer proton therapy.
How can you use this information?
BE THE CEO OF YOUR OWN HEALTH – Take simple steps if your cancer is in the chest region:
- Ask your doctor “what is my mean heart dose?” – if it is not close to 1Gy or less – you might benefit from protons
- Ask your doctor if you have calcium in your heart arteries on your planning scan – or ask if your CAC score is 0.
- Ask your doctor what the dose is to your LAD or what metrics they use to judge dose to the LAD?
- And then, exercise, eat healthy, don’t smoke.
Simply by asking these questions, you’ve probably helped reduce the dose to your heart. By taking care of yourself and living heart-healthy, you’ve taken another step forward.
Be an advocate for your own health – ask questions and understand your treatment options. Cardiac toxicity following radiation is a known event. It is modifiable and there is growing information that proton therapy can reduce heart damage.
Dr. Mark Storey, MD
Medical Director Oklahoma Proton Center